Many older adults seek to do one thing as they advance in age: spend their later years in a familiar and comfortable environment — in their own home. This is an important goal, and it highlights a strong preference for maintaining independence and familiar surroundings rather than transitioning to assisted living facilities or nursing homes.
Nevertheless, some older adults, hindered by health issues, are unable to reach this goal because of frailty—a condition that can be mitigated if not prevented with the right steps.
Frailty’s ongoing impact
Frailty, often found in older adults, increases the risk of hospitalization, prolonged hospitalization, readmission, falls, cognitive decline, and functional decline.
Frailty is characterized as a combination of problems:
- Weakness
- Fatigue
- Decreased strength
- Poor balance
- Unplanned weight loss
Taken individually or as co-morbidities, these challenges make it difficult for an older adult to recover from an illness or injury. Unfortunately, frailty is often difficult to identify and manage.
Preventing or reversing frailty and avoiding the factors that lead to hospital admissions can result in improved recovery, health, and independence.
Older adults by the numbers
The average cost of hospitalization can be as high as $11,900 for seniors. The number of Americans ages 65 and older is projected to increase from 58 million in 2022 to 82 million by 2050 (a 47% increase), and the 65-and-older age group’s share of the total population is projected to rise from 17% to 23%. Nearly 95% of older adults have at least one chronic illness, according to the National Council on Aging. Seniors account for more than 40% of hospitalizations each year for chronic illnesses, fall-related injuries, surgeries such as joint replacement, and other health problems.
Hospitalizations often lead to a disruption of daily activities, reduced mobility, skin breakdown, cognitive decline, loss of independence, and other issues. A Yale study indicates that “Frail patients were readmitted within 180 days at a rate of 36.9%; patients with probable dementia were readmitted at a rate of 39%; and patients 90 years old and older were readmitted at a rate of 36.8%.”
Hospital readmissions carry a heavy financial burden of over $50 billion annually.
In many cases, these readmissions are avoidable. Readmissions may be attributed to the quality of care received during hospitalization, inadequate self-care or caregiver support post-discharge, lack of follow-through with appointments and treatment (including medication reconciliation), and other factors.
Common factors impacting rehospitalization for seniors include older age, poor socioeconomic status, malnutrition, multiple co-morbidities (particularly heart failure, frailty, liver disease, and anemia), and prolonged hospitalization. There are also factors unique to each individual, such as cognitive decline, chronic conditions, fall history, current quality of care and related care coordination, social support, understanding their specific needs and adherence to the treatment plan, the length of the initial hospital stay, and discharge timing.
Exploring health data for a better life
Common misconceptions about data analytics often include the need for large amounts of data, only needing to do analysis once, or that a high-tech solution is required. Asking the right questions in a simple survey of the population can yield a tremendous amount of information. The important question in this case with older adults: What does our population need to avoid readmission to the hospital?
Health indicators, medications, care plans, and other data are used to analyze and identify trends in readmission rates and risk factors. These trends can be leveraged to pinpoint the areas where interventions could have the most impact. The data can also be utilized to personalize interventions, address the unique needs of each member and coordinate care, and enhance communication.
Beyond numbers and data
While data and cost are important elements in recognizing issues, the measure of success isn’t just about the data or the numbers; it’s about ensuring that older adults can manage and maintain their expectations about health and aging in place.
For older adults, choices related to healthcare, lifestyle, and activities of daily living should align with quality of life, independence, and emotional well-being.
Maintaining good health and a sense of autonomy can enhance longevity, reduce healthcare costs over time, and support mental and emotional resilience. A holistic healthcare approach ensures that older adults receive not only effective medical care but also the emotional and social support necessary to lead fulfilling lives.
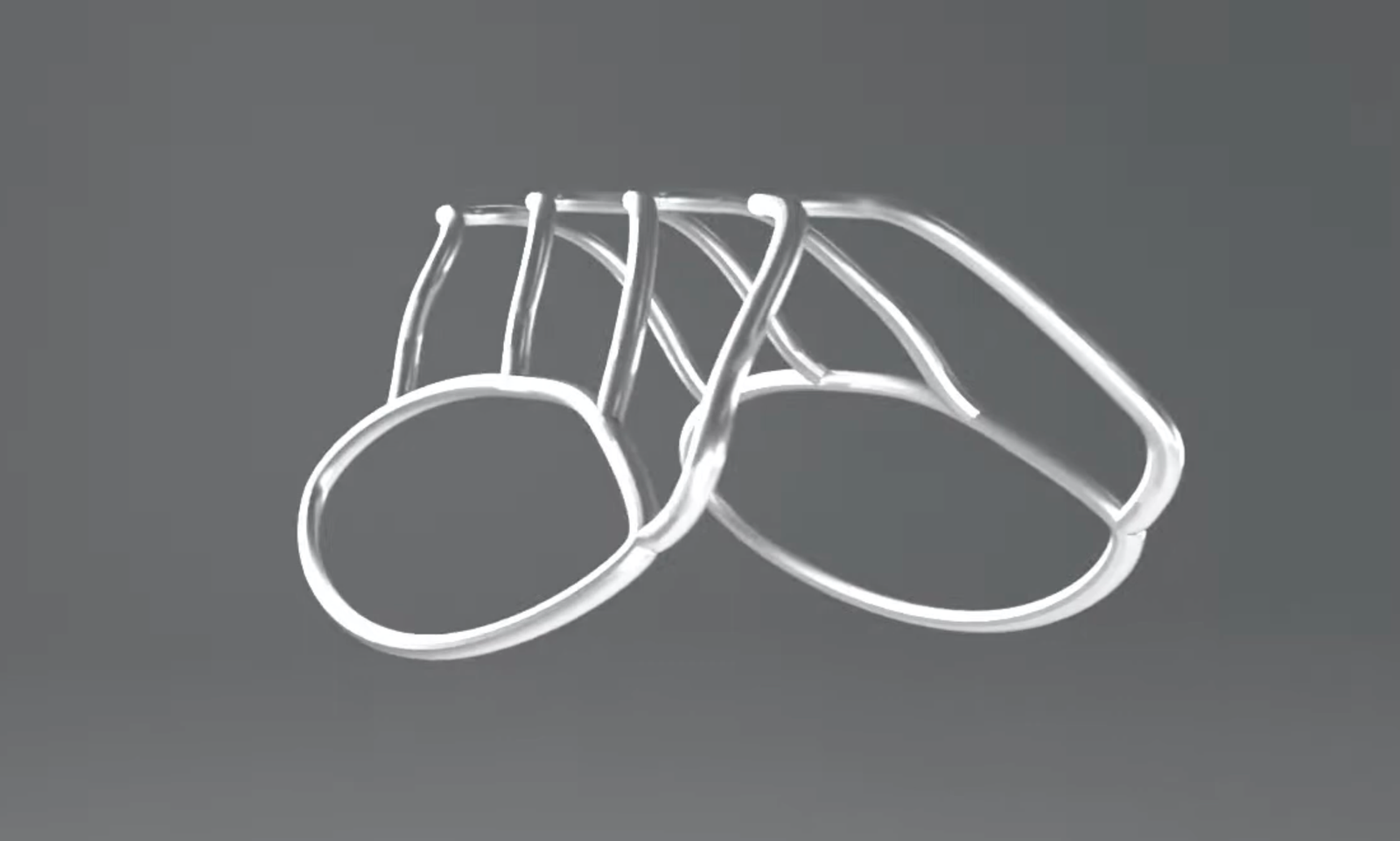
Comprehensive aging-in-place solutions, backed by evidence-based guidelines, include screenings and assessments for frailty and fall risks, identifying the root causes of risk factors, and providing effective interventions to modify risk factors to help older adults build resilience. Older adults participating in an aging-in-place program can expect to live a functionally independent life at home while developing resilience for the future. Health plans may discover that addressing frailty and falls through a comprehensive program leads to a reduction in total care costs and an improvement in Star Ratings.
Effective aging-in-place programs include innovative, clinically evidenced, multi-domain, and technology-supported interventions. An effective support program includes:
- A dedicated care manager with education and experience in helping people find new ways to live safely at home
- Ancillary team members, including pharmacists, social workers, nurses, occupational therapists
- A coordinated effort to provide supportive education, referrals to appropriate and vetted service providers, such as home modification companies or caregiver services, and provider coordination support
- An omnichannel communication approach that honors the member’s preferences, which may include a website, an app, bi-directional digital communication tools such as texting and email, and asynchronous phone and education campaigns
- A whole-person care philosophy to engage members in a positive, collaborative experience while reducing and averting risks associated with frailty, falls, and unplanned hospitalizations
We in healthcare have a significant opportunity to help older adults by bringing together data, personal surveys, and one-on-one interactions, while recognizing that behind every number and data point is a person with unique expectations and aging-in-place goals.
Photo: izusek, Getty Images

Krithika Srivats is Senior Vice President of Clinical Practice and New Products & Solutions at Sagility. She is passionate about geriatric care and has implemented several innovative elder resilience programs in many countries. She leads the Smart Step Aging in Place Program at Sagility.
This post appears through the MedCity Influencers program. Anyone can publish their perspective on business and innovation in healthcare on MedCity News through MedCity Influencers. Click here to find out how.